As the worldwide number of COVID-19 cases surged past the 1 million mark on April 3rd, one-third of the global population is currently under lockdown in an attempt to quell the spread of the novel coronavirus. While countries with advanced economies are either coming out of the height of their own pandemic (e.g. China) or are in the midst of their battle against a surge of cases (e.g. U.S., U.K.), most low- and middle-income countries (LMICs) are only at the beginning of their coronavirus fight. Lockdowns are dramatically changing everyday life in LMICs across Africa, Asia, and Latin America, where shelter-in-place orders are becoming synonymous with loss of daily wages and heightened food insecurity.
Whether the slow spread of coronavirus in LMICs is due to temperature and climate patterns, reduced air travel routes to and from such regions, or the limited testing and monitoring capabilities, one thing that can be agreed upon is the inability of the healthcare systems of most LMICs to bear the weight of the coming COVID-19 burden. The indicators that expose fragile health systems in the face of a global pandemic are cause for concern. India has 0.5 hospital beds per 1,000 people and has tested fewer than 30,000 individuals out of its 1.3 billion population. Nigeria has approximately 75,000 registered health professionals, with few intensivists trained on ICU care and ventilation, and only five laboratories able to test for coronavirus. Indonesia, with one-sixth the per capita number of doctors as South Korea, already holds the highest coronavirus death rate at 9.2 percent compared to a worldwide average of 5.2 percent.

The dire circumstances of LMIC health systems make it obvious that LMICs’ COVID-19 response cannot take the same path as their advanced economy counterparts. Even if governments and donors were to somehow conjure up the funds today, the massive healthcare infrastructure and human capital investments required to save thousands of additional lives would never be ready in time for the imminent flood of coronavirus cases in the coming weeks. Concerted action must be taken now. But how? A feasible COVID-19 response in resource-constrained settings would have to center on providing the means for vulnerable populations to eat under lockdown, coupled with massive behavioral health information campaigns.
A range of COVID-19 response approaches have been taken by countries around the world. The U.K. toyed with a do-nothing “herd immunity” approach before rightly backing away from this doomed approach on March 23rd. Although Africa’s young median age of 19.7 years may seem like an argument in favor of doing nothing in the face of a virus that disproportionately targets the elderly, the double burden of disease LMICs face gives pause to think again. LMICs face high rates of infectious diseases like tuberculosis and malaria, but also an increasing rate of non-communicable diseases such as cardio-vascular diseases, cancers, and chronic respiratory disease. Letting the virus spread uncontrolled would place millions of lives at risk—the aged, the vulnerable, and the seemingly young and healthy.

Lauded throughout the world as success stories for COVID-19 response, Singapore and Taiwan’s aggressive testing, tracking, and containment approaches have been highly effective thus far. Early in the worldwide outbreak, Taiwan quickly devised travel and disease control policies. It made use of a comprehensive database with real-time information on patients, symptoms, and treatment. These are commendable actions Taiwan can financially afford to take, given its 2017 GDP per capita of $57,714. Unfortunately, with a comparable GDP per capita between $300 and $4,000, most LMICs don’t have the testing and monitoring resources to effectively replicate a test-track-contain based response.
Though the world was stunned and initially critical of China’s perceived draconian measures to shut down Wuhan and many nearby cities, it is now widely accepted that travel bans and lockdowns are effective containment tools for reducing the spread of the virus. Though most experts note they were late to enact lockdowns, France, Italy, and the U.K. are among the higher income countries that have implemented the most wide-spread and restrictive quarantine measures in a bid to flatten the curve. Coupled with the quarantines are measures to provide financial assistance to individuals and industry. Many European governments have stepped in to pay wages, with governments spending billions on wage subsidies in order to save jobs and ease the economic fallout. The U.S. is using a $2 trillion stimulus bill to provide cash and assistance to individuals, businesses, and hard-hit industries in the face of its lockdown. The emergent consensus among health experts and governments is when strongly implemented and adhered to for sufficiently long periods of time, lockdowns work.
In most LMICs, the feasibility of strict lockdowns must be assessed under a completely different lens than what is seen in advanced economies. Over a quarter of the world’s population—1.9 billion people— live on less than $3.20 a day, many of whom reside in LMICs. These are often countries with some of the largest slum populations, making social distancing and self-isolation far-fetched ideals unsuitable for the average person’s living conditions. The large proportion of people in LMICs working within the informal economy as street hawkers, tailors, and market merchants are quickly made vulnerable to financial and food insecurity when placed under lockdown. Moreover, migrant remittance flows, which are equivalent to 80 percent of the federal government budget and 11 times foreign direct investment flows in Nigeria, have already dropped significantly from top “send” countries in the West under lockdowns. Additionally, many amongst the most impoverished populations do not have easy access to soap and clean water necessary for virus-killing handwashing, or they believe that coronavirus is a disease limited to foreigners and the affluent, a rich man’s disease. LMICs must grapple with the fact that coronavirus is lethal, but so is poverty.

How might LMICs begin to flatten of the curve with lockdowns while sufficiently supporting the economy? Resource-constrained countries must develop methods of providing social safety nets—predominantly food security—while enacting national quarantines and mass media informational campaigns.
The stimulus packages—which lie in the range of 10 percent of GDP— that have been coupled with quarantine measures in advanced economies are fiscally unfeasible for most countries across Africa, Latin America, and parts of Asia. The recent drop in the price of commodities such as crude oil and copper, whose proceeds constitute the majority for foreign exchange for a number countries, further limits the funds and resources available to tackle COVID-19
Although not as impactful as large stimulus cash infusions, feasible alternatives for LMICs are beginning to emerge. Early this week, Zimbabwe budgeted over $600 million to protect one million vulnerable households through a cash transfer program. Nigeria has announced financial intervention schemes to be rolled out for vulnerable populations, with Lagos state and other states beginning state-level interventions. India has announced a $23 billion relief package to help the 94% of the country’s population employed in the informal industry. On top of this, many philanthropic organizations have created paths for charitable giving and philanthropic donations aimed at direct citizen-to-citizen cash and goods allocations.
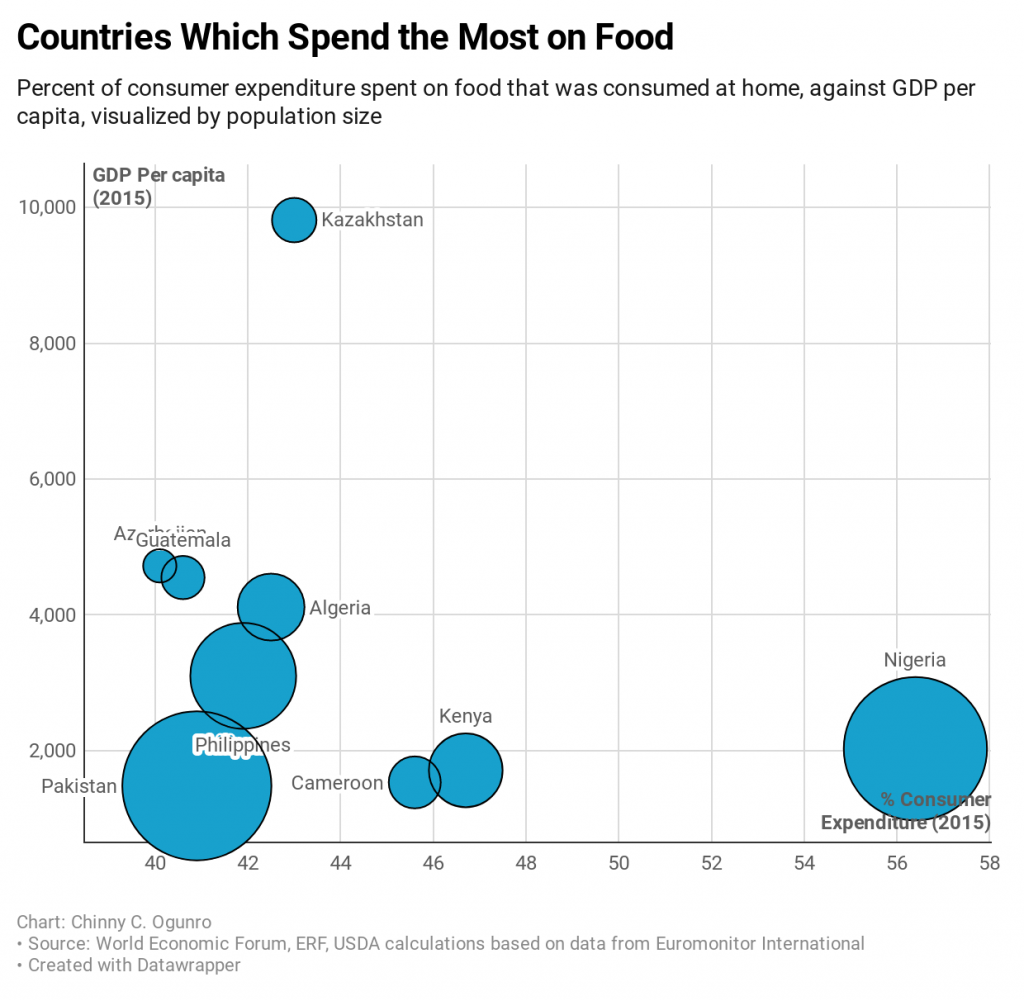
These early safety net efforts are a good start. However, the immediate issue of food insecurity stemming from the loss of daily wages cannot wait for transfer programs that may take weeks to materialize. Nigerians spend up to 56 percent of their income on food, a significant amount compared to the meager 6 percent spent in each the United States and Singapore. To be able to enact the likely long-term, periodic quarantines that are required to defeat COVID-19, more immediate formal means of providing basic food and water are necessary. Measures must be taken to ensure that farmers and workers in the food industry are adequately supported and LMICs medium- and long-term food supply chains are secured. Safe and uncrowded methods for getting food to households must be put into place.
For the minority high-income earners within LMICs, keeping food markets open and setting strict guidelines on how many can enter at a given period of time is likely sufficient. To feed the low-income masses, we need government and donor support of key stakeholders in the food and agriculture industry, as well as ways of guaranteeing players along the food value chain adhere to strict safety and health protocols. As a reasonable example, on April 4th Uganda began food relief distribution to 1.5 million urban poor affected by the lockdown. To reduce the risk of transmission from gathering crowds, bags of rice, beans, and salt are delivered door-to-door by military personnel from food trucks. This method supports vulnerable populations’ ability to shelter-in-place by ensuring access to basic foods.

The long-term viability of LMIC health systems and the development of their broader economies will depend on whether they successfully navigate the precarious waters that CCOVID-19 has thrown them into. Surface-level replication of responses taken in advanced economies are not enough. To battle both coronavirus and poverty, concerted and conscientious effort must be made to provide sufficient safety nets and secure daily access to food.





